|
Too often a child’s body is restored to health in the hospital, but the child is sent home with emotional wounds. This study explored the needs of children in a haematology-oncology unit as well
as the resources that could be mobilised in order to address these needs by firstly carrying out a literature review. A field studywas then conducted in order to prioritise the resources according to
their importance for children in a haematology-oncology unit. A definite trend could be found in the way that the children responded to the request to prioritise the resources. The first three resources,
as chosen by the children, all concerned the external social environment of the child. It could therefore be concluded that support from parents and other people of significance are most important to the
child and should betaken into account when facilitating support for children in a haematology-oncology unit. It could also be concluded that these children do not experience sufficient control in their
situation and it could therefore be suggested that children in a haematology-oncology unit should experience more control and power in their situation.
So dikwels word ‘n kind se liggaam genees in die hospitaal, maar hierdie selfde kind gaan huis toe met emosionele wonde. Die behoeftes van kinders in ‘nhematologie-onkologie eenheid is ondersoek
asook die hulpbronne wat gemobiliseer kan word om hierdie behoeftes aan te spreek deur gebruik te maak van ‘n literatuurstudie. Daarna is ‘n veldstudie gedoen om hierdie hulpbronne te prioritiseer
volgens die belangrikheid daarvan vir kinders in ‘n hematologie-onkologie eenheid. Die manier waarop die kinders die hulpbronne geprioritiseer het, het ‘n definitiewe tendens getoon. Die eerste
drie hulpbronne wat deur die kindersgekies is, is al drie hulpbronne wat die eksterne sosiale omgewing van die kind behels. Die gevolgtrekking kan dus gemaak word dat die ondersteuning van ouers en ander
persone wat belangrik is vir die kind, van uiterste belang is en in aanmerking geneem behoort te word in die fasilitering van ondersteuning van kinders in ‘n hematologie-onkologie eenheid. Die
gevolgtrekking wat gemaak kan word is dat hierdie kinders nie genoeg beheer ervaar in hulle situasie nie en daarom wordvoorgestel dat kinders in ‘n hematologie-onkologie eenheid meer bemagtig
behoort te word gegewe hulle omstandighede.
Any hospital stay contributes to high levels of stress for children as they are often subjected to negative and unfamiliar stimulation from the environment and that stress could threaten their well-being
(Gaynard et al. 1998:16). The admission of a child to hospital is very stressful for the child because of various reasons, including the fact that normal fears and fantasies of the child could be
intensified (Potts & Mandleco 2002:459). The insecurity of hospitalisation were mentioned as a majorstressor for children with cancer by McCaffrey (2006:62) and one child was quoted as saying:
‘Hospital is a shock coming in’ and ‘I don’t look forward to coming in here, it is just different’. With a haematology-oncology diagnosis, children are
repeatedly subjected to the hospital experience that could lead to a sense of ‘profoundly altered normalcy’ by the whole family (McGrath 2001:232). Battles and Wiener (2002:65) stated that children with a chronic illness often have to cope with ‘repeated hospitalizations, invasive procedures, physical discomfort, side effects of medication,
and the potential for a shortened life expectancy’. Phipps et al. (1998:148) described the invasive procedures that children undergoingoncology treatment so often have to face as an
‘uncontrollable, acute stressor’. Levine and Kline (2007:198) explained that a person’s natural reaction towards a stressor is to fight it or flee from it but if that is not possible,
as in the case of invasive procedures, it has the potential to overwhelm the person, that is, the child. Children cannot always understand the side effects of the treatment because they usually feel
quite well when diagnosed and experience the treatment as much worse than the illness (Van Dongen-Melman & Sanders-Woudstra 1995:31). Steward et al. (1996:106) warned that ‘the diagnosis
and treatment of childhood cancer present children with experiences falling well outside the normal range, and well beyond the parameters of most children’s coping repertoires’. According to
Hobbie et al. (2000:4060) this experience can lead to post-traumatic stress symptoms in adult survivors of childhood cancer, including avoidance, heightened arousal as well as
re-experiencing the trauma which in turn can cause the person to avoid medical care and follow-up.
Problem statement
In South Africa, 700 children are annually diagnosed with some kind of malignancy (Cutland 2004:39) whilst Patenaude and Kupst (2005:9) stated that three out of four children diagnosed with a malignancy
are expected to survive the disease. McCaffrey (2006:59) warned that it is important to render ‘skilled supportive care’ to children and families in a haematology-oncology unit, but in order
to do this, the needs of these children should be continuously evaluated and taken intoconsideration in planning supportive care. Von Essen et al. (2002:601) cautioned that the nurse cannot rely
on intuition when deciding on which aspects of support are needed most by children in a haematology-oncology unit and therefore the following research questions were asked:
• What are the needs of children in a haematology-oncology unit?
• What are the resources that can be mobilised so that the needs of these children can be met?
• What aspects of support are needed most by these children?
Aims of the study
The aim of this research was to identify the needs of children in a haematology-oncology unit and to identify and prioritise resources that could be mobilised in orderto meet the needs of these children.
Significance of the study
The purpose of the field study was to prioritise the different resources identified in the literature review according to their importance for children in a haematologyoncology unit. The following 19
resources were identified during the literature review and prioritised by the children during the field study:
• support in handling the side effects of treatment. The most prominent physical side effects of children with a haematology-oncology diagnosis were identified as body changes, eating problems and inadequate
sleep and therefore the resources that will be explored are as follow: support with eating problems and support with inadequate sleep. Body changes will not be included as a resource seeing
that other resources such as ‘information’ and ‘support from friends’ were found effectivein supporting the child with body changes according to the literature review.
• support in coping with pain
• support with schoolwork
• alleviation of misconceptions and the provision of adequate information
• play interventions
• humour as intervention
• music interventions
• tokens of appreciation and encouragement
• literature
• electronic devices
• the promotion of control
• religious activities and spiritual support
• the reduction of negative sensory stimulation from the environment and the normalising of the environment
• support from parents and family. This resource will be divided into two aspects to make it easier for the child to prioritise, namely support from parents and support from siblings.
• support from friends
• the establishment of a trusting relationship
•animal assisted activities.
Literature review
The literature was explored and references were made with regard to the needs of children in a haematology-oncology unit. Furthermore, the resources that arecurrently used in healthcare and that could address the needs of these children were identified. Resources used to support general paediatric patients across the world were also investigated in order to determine if they could meet the needs of children in a haematology-oncology unit. Literature in the medical and nursing fields as well as in other relevant fields (such as child life, sociology, psychology and education) was explored by using keywords such as: ‘child life’, ‘children’,‘hospital’, ‘haematology-oncology’, ‘support’, ‘resources’ and ‘needs’. An explorative and descriptive research design was used during this phase by exploring relevant literature and describing the needs of children in a haematologyoncology unit as well as the way in which the resources that were identified, address the needs of the children in a haematology-oncology unit. The Theory for Health Promotion in Nursing (University of Johannesburg: Department of Nursing Science 2010:4) were used to classify these needs and resources (Table 1). According to this theory, the child is seen holistically and in interaction with the environment in an integrated manner, where environment implies an internal aswell as an external environment. The internal environment consists of body, mind and spirit dimensions whereas the external environment consists of physical, social and spiritual dimensions.
|
TABLE 1: The needs of children in a haematology-oncology unit and the resources intending to meet those needs.
|
|
Research method and design
|
|
Design
During this study, an explorative, descriptive and contextual research design was used. Very little research has been conducted on the needs of children in ahaematology-oncology unit and the different
ways of meeting these needs; therefore this field was thoroughly explored during a literature review. After the literature review, results were described according to the different needs of children
admitted to a haematology-oncology unit as well as various resources that could be mobilised as a way of addressing the needs identified. The next step was to explore these resources further through a field study in order to prioritise the different resources identified in the literature review in accordance with their importance
to the children. In order for this study to be relevant and applicable in practice, the research was conducted in the context of haematologyoncology healthcare in the private sector in South
Africa and a description was given of the context (see Context of the study).
Population and sampling
All children who have been treated in a private hospital in the Tswane metropolitan area and who met the inclusion criteria were contacted and included in the research if it was possible for their parents
to bring them to the meetings. Individual meetings were held with the children outside the hospital at a time when they were not hospitalised. The inclusion criteria were as follow (Table 2):
• Primary school aged children, implying children from the age of six years up to 13 and even 14 years, with the provision that they were still in primary school and that they have received
active treatment before the age of 13 years. Children of this age group are able to sort items systematically according to specificcharacteristics, given that they are able visually see the items
(Cook & Cook 2005:249). It is also important to note that Von Essen et al. (2002:608) stated that ‘all aspects of care reported as important for children aged 8–12 years and
being treated for cancer were found also to be important for children aged 0–7 years’.
• The parents of the children must have been willing to consent to the study and bring the child to the meetings, and the child had to give his or her assentvoluntary. This implies that all
relevant information was given to the child as well as to the parents (Abramovitch et al. 1995:26, Range & Cotton 1995:49).
• The children must have been treated previously for an oncology or haematological disorder in one of the private paediatric haematology-oncology units in the Tswane metropolitan area.
They must have been admitted to the hospital during the previous six months before the meeting with the researcher, either for activetreatment or for follow-up procedures if they were in
remission. McDermott Sales et al. (2005:543) as well as Alexander et al. (2005:38) concluded that children are able to recall stressful and emotional experiences years after
it happened. Steward et al. (1996:115) referred to another study that investigated children’s memory of invasive procedures and found that their reports and judgement of the
procedure were accurate and complete even after six months. It could be concluded thatchildren would remember their hospital experience, especially because the memory would have been
reinforced every time that the child had to visit the hospital for follow-up procedures.
The names of the children were obtained from the Childhood Cancer Foundation of South Africa (CHOC). All children meeting the above criteria were included in the study, irrespective of their diagnosis. The only children that were excluded from the study were childrenthat have been treated for a
brain tumour. According to Patenaude and Kupst (2005:14–15), children with brain tumours are at an increased risk for psychosocial cognitive behaviour as well as adjustment disorders.
Consequently they are as a rule excluded from psycho-oncology research because their experiences differ so much from that of the majority of children receiving haematology-oncology treatment.
Ultimately, 26 children participated in the study and saturation of data wasobtained as the same trend for prioritising the data emerged repeatedly.
|
TABLE 2: Background variables of the children in a haematology-oncology unit.
|
Data collection methods
In order to prioritise the different resources identified in the literature review according to their importance for the children, an adapted Q-sort method was used.This method involves ‘a technique
of comparative rating that preserves the subjective point of view of the individual’ (Burns & Grove 2009:414). It is suggested that 40–100 cards with a single phrase or picture on each card
are presented to a participant, whereupon the participant is asked to sort these cards in seven to 10 different piles according to the importance or priority assigned to them by the participant (Burns &
Grove 2009:414). For the purpose of this study, however, and in view ofthe ages of these children, only 19 cards were used and the children were asked to sort it in only three categories. Different cards were developed that portrayed the resources identified from the literature review as full-colour pictures. A phrase describing the specific resourcewas written on the card in either
Afrikaans or English. These cards were merely used as icons, implying that each card signified a specific resource by virtue of resemblance. This is in accordance with the taxonomy of types of signs
by Charles Sanders Peirce (1839–1914) as explained by Siegel (1995:455 & 2006:68). The children were therefore not asked to interpret the cards and each card was explained to the children
to ensure that they understood what each card resembled. Individual meetings were held with the children in locations most convenient for the families and although the meetings took place in different locations, the direct environment of the child was kept
as uniform as possible. Parents were not present during the meeting with the child because they might have influenced the child’sdecisions (Morison, Moir & Kwansa 2000:117). Although the room
in which the meetings were held was different with each interview, the child sat at a table with the pictures arranged in front of him or her in exactly the same way for the sake of consistency. The
pictures had a small number at the back of the picture that the child was unaware of so that the researcher was able to arrange the pictures in the same way. The children received the cards resembling
the resources with the descriptivephrase in either Afrikaans or English, according to their language of preference. The pictures were separately mounted on A5-size cardboard so that the children could
move the pictures around and sort them in a box with three separate compartments. In the top compartment were those resources that they regarded as the most important, in the second compartment were
those that were less important, and in the last compartment were the rest of the resources that they would regardas the least important. According to Woods and Catanzaro (1988:327) the number of cards
placed in each compartment should be specified by the researcher, but the distribution of these cards are open for the researcher to determine. In the current study, the researcher assisted the children
in this regard in order to distribute the cards evenly between the three compartments, implying between six and seven cards in each compartment. The researcher examined all the cards with the child to make sure that the child understood what each picture and description represented. She explained to the child what to do and how to sort the cards
in the different compartments as described and then asked the same opening question to each of the children: ‘What do you think would be the most important thing for a child in hospital to make the hospital a better place? Imagine a white room and a white bed with no-one and nothing there. Which of these things [referring to the cards in front of the child] should be there first?’ (Researcher) The researcher made no further comments during the meeting, except when it was necessary to encourage the child to carry on with an ‘and then’ remark. The researcher only intervened
if a child placed too many cards in one compartment, but did not assist the child by any means to make decisions during the meeting,not showing any signs of approval, disapproval or surprise at the
child’s decisions at all. A child is very sensitive to the reactions of the interviewer and this could influence a child’s responses (Kortesluoma, Hentinen & Nikkonen 2003:440). At the
end of the meeting, the researcher recorded the order in which the child sorted the resources (see Data analysis) and any additional remarks that the child might have made during the interview were
written down.
Data analysis
The resources as sorted by the children were scaled based on Woods’s and Catanzaro’s (1988:326) suggestion that the Q-sort method can also be used as a scalingtechnique. Scaling implies
‘the construction of an instrument that associates qualitative constructs with quantitative metric units’ in order to measure abstract concepts and to assign a number to these concepts
(Trochim 2006). Different numerical values were therefore assigned to the resources according to the way in which the resources were sorted by the children: high importance received three points,
medium importance received two points and low importance one point. The numericalvalues of each resource were added up and divided by the number of children who prioritised that specific
resource in order to determine the mean score for each resource (Table 3). The two children who had no siblings did not receive a card for support for siblings. Consequently, the resource,
support for siblings, was only prioritised by 24 children and not by 26 as the other resources were and the values that were added up was therefore divided by 24 in order to determine the
meanvalues (Figure 1). Descriptive statistics were used to describe the priorities as obtained from the children, further.
|
TABLE 3: Results of the scaling of resources compared to the internal and external environment of the child.
|
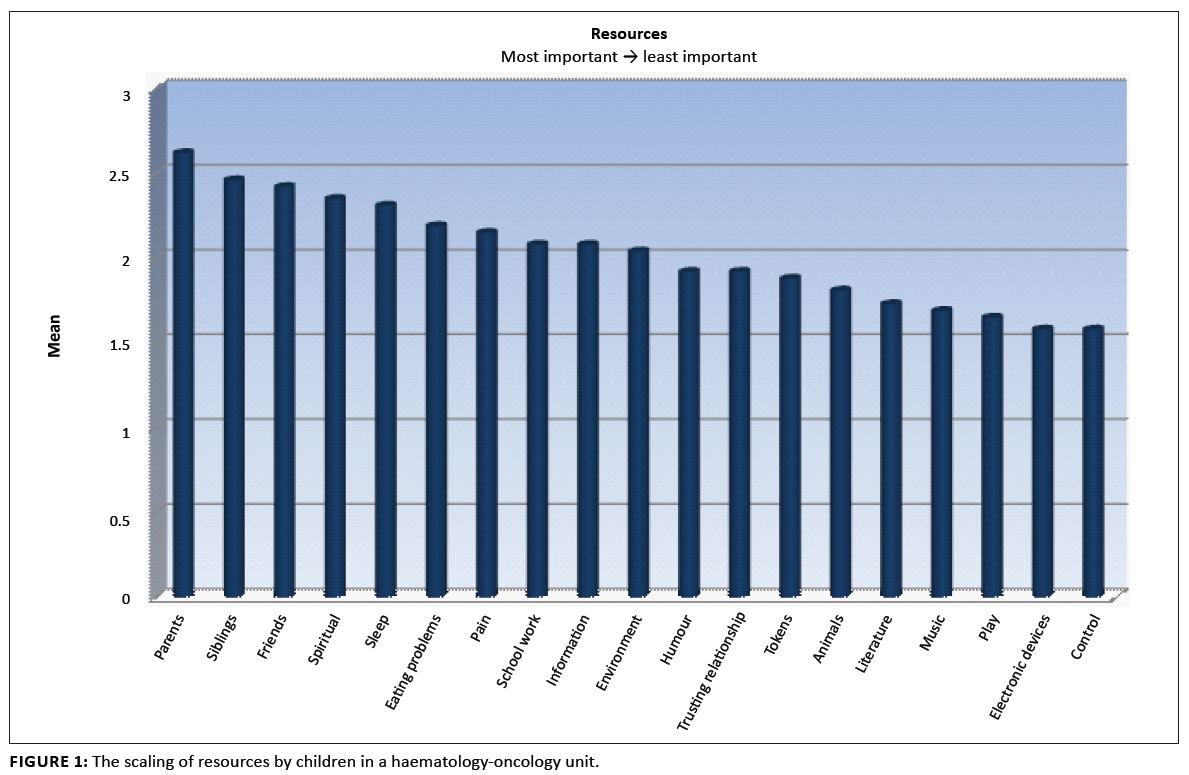 |
FIGURE 1: The scaling of resources by children in a haematology-oncology unit.
|
|
Context of the study
Children being treated in a haematology-oncology unit in the private sector were chosen because financial and other resources are readily available and the resources can be optimally explored. Although
the needs of children from both the private and the public sector should be explored, it is not possible to include both in thesame study. In the private sector parents or caregivers are usually
available most of the time during a child’s hospitalisation, whereas in the public sector children are often left alone as a result of the high incidence of single parent household and
transport problems when children are treated long distances from their home. In private hospitals, the interior decorating is usually child-friendly and colourful and designed by professionals,
which is not always the case in the public sector.Televisions and other electronic equipment are also more readily available in private hospitals (Van Dalen 2008). This could all lead to different
needs from children hospitalised in the private healthcare sector and those in the public sector. After the needs of children in a haematology-oncology unit in the private sector have been explored
and described, the needs of children in a haematology-oncology unit in public hospitals should be explored as well as the resources that could address those needs. This was, however, not part of the
current study.
Nolan (1996:64) explained that the Medical Research Council of the United Kingdom proposed guidelines specifically for research with children and proposed that research on children is only justified if:
• the same information could not be obtained from adults
• it is approved by the local research ethics committee
• consent has been given by either the child or his or her guardian and the child does not object or appear to object to the research (also referred to as assent), and noharm will come to the child.
During this study, all the above guidelines have been adhered to. The research has also been approved by the Academic Ethics Committee of the Faculty of HealthSciences of the University of Johannesburg.
According to Burns and Grove (2003:201) bias can be prevented during a descriptive research design by applying certain measures:
Conceptual and operational definitions of variables: The resources were identified by thoroughly exploring the literature and a detailed description of each of theresources was given.
• Sample selection: A purposive selection of cases was used. All the children of primary school age who have been treated in a private haematology-oncology unit in the Tshwane metropolitan
were included in the study as far as possible in order to ensure that children who have been diagnosed with a haematologyoncology disorder are well represented in the study.
• Valid and reliable instruments: In order to ensure content validity, all the resources were determined by means of a thorough investigation during the literature review and a detailed description
of each of the resources was given. These resources were prioritised according to the adapted Q-sort method. This method hasbeen used extensively in nursing research in the past (Woods &
Catanzaro 1988:326). Children need to see items in order to sort these items (Du Toit & Kruger 1991:118); therefore it is important to make use of pictures as visual aids. The pictures were
only used as icons resembling the resources in order to guide the child and to make it easier to identify the different resources Siegel (1995:455 & 2006:68). Steps were also taken to ensure
reliability. During the individual meetings,the same instrument was handed to all the participants in the same way by the same person with the same research question posted to all of them. A pilot
study was also conducted in order to clarify the opening question and to determine whether the children were able to follow the instructions as this also added to the reliability and validity of the
study (Kortesluoma et al. 2003:440).
• Data collection procedures that achieve some environmental control: Although the environment will be different with each meeting, it will be kept consistent and as relaxed and child-friendly as
possible (see discussion under ‘Data collection’).
The different needs of children in a haematology-oncology unit and the resources that could be mobilised in order to meet these needs as identified in the literature review are summarised in Table 1.
The classification of these needs and resources were carried out according to the categories of internal and external environmentas proposed by the Theory for Health Promotion in Nursing
(University of Johannesburg: Department of Nursing Science 2009:4). Some of the resources could fit into more than one category, but were only sorted in the category that is the most relevant. A summary of the results of the field study are depicted in Table 3 and Figure 1. Each of the resources will now be discussed briefly according to the priorities as assigned by the children.
Priority 1. Support from parents (external environment–social)
Gaynard et al. (1998:85) explained that children rely on parents and family members to fulfil their physical, emotional and intellectual needs and that they will host feelings of abandonment
in the absence of their parents or significant others. They also made it clear that parents are an important link between healthcare providersand the child, given that they are better able to explain
what is happening to the child and to give the child the relevant information as needed. Parents also help to make the environment more familiar to the child and provide a sense of security. It is
therefore vital that parents are included as part of the healthcare team. Even when adolescents were diagnosed with cancer, their parents (and especially their mothers) were found to be their most
important source of support (Woodgate2006:127).
Priority 2. Support from siblings (external environment–social)
The Child Life Council (1997:49) declared it ‘highly desirable’ for siblings to visit their sick brother or sister in hospital and according to Slade (2000:112), these visits are
important in order to maintain family relationships and to help the sibling understand the nature of the illness and treatment (Table1). Siblings were rated more important than friends, which
is the next priority. Gizynski and Shapiro (1990:190) agreed and explained that the child with an oncology diagnosis were ‘morecomfortable and less anxious with family members than peers’.
Priority 3. Support from friends (external environment–social)
As the third highest priority, it is clear that these children need the support of their friends. Positive interactions with healthy peers could be beneficial for the child (Derevensky, Tsanos &
Handman 1998:42,54) and they should be encouraged to visit the child in hospital although they should also be cautioned not to treat the child differently because of the cancer diagnosis (Woodgate
2006:126). Social interaction between patients in the ward is very important and should be encouraged(Meltzer & Rourke 2005:307,311). Gaunt (1993:35) added that for this reason hospitalised
children should be admitted in communal wards rather than in single rooms.
Priority 4. Spiritual support (internal environment–mind–spirit)
According to Gaskill (2001) it is important that if a child is used to certain religious practices such as mealtime prayers and bedtime prayers, these practices should be maintained during hospitalisation
(Table 1). Gaskill also warned that it is vital to ensure that children do not see hospitalisation as a punishment for misbehaviourand to assist them to deal with feelings of anger or guilt. Spiritual
support can be seen as a high priority for the child in a haematology-oncology unit and this is also confirmed by Malan (2003:126) who speculated that the illness itself might be a motivation for both
the child and his or her parents to become more religious.
Priority 5. Support with sleep (internal environment–body)
Carver and Scheier (1996:414) explained that the need for food and sleep are basic needs and these needs are ‘deficiency-based’, implying that the need will be met through trying to avoid
unpleasantness such as a lack of sleep or nausea. This might explain the reason why the children chose adequate sleep and enjoyable dietas the fifth and the sixth priority. The need for support with
sleep can be addressed by reading children a bedtime story (Burke, Kuhn & Peterson 2004). White et al. (1990:138) also found that a story with the suggestion to fall asleep was beneficial
in reducing anxiety and decreasing the length of time to fall asleep. They further suggested that nurses should implement a specific bedtime for patients in a paediatric unit when the lights are to be
dimmed, noise levels reduced, televisionsswitched off and stimulating activities discontinued well in advance of the scheduled bedtime.
Priority 6. Support with eating problems (internal environment–body)
Armstrong (1992:211) regarded nausea and vomiting as acute aspects of oncology treatment and stated that it should receive prime focus in the care of children. Relaxation, guided imagery as well
as distraction have all been used successfully to control chemotherapy-induced nausea and vomiting in children and, as a result, increased treatment compliance. It is, however, important to teach
the child the necessary skills to cope with the problems before they arise so that anxiety anddistress can be eliminated and self-esteem and quality of life promoted (Kaufman et al. 1992:21,
Oncology Nursing Society 2005). Interactive persuasive games can also be used as a distraction and to encourage children to eat (Lin et al. 2006).
Priority 7. Support in coping with pain (internal environment–body)
According to Twycross, Moriarty and Betts (1998:6), children often deny the fact that they have pain; one of the reasons for this is that they believe that they have to be brave and this might have
prevented the children from rating coping with pain as an even higher priority. Support in coping with pain should be a primary focusin a haematology-oncology unit (Armstrong 1992:211). Besides
pharmacological measures for managing pain, the following interventions are successfully utilised in healthcare to reduce pain:
• distraction (Twycross, Moriarty & Betts 1998:96; Petrovic et al. 2000:19)
• relaxation (McGrath, Dick & Unruh 2003:303; Liossi 2002:117)
• by holding a child in a comfortable (mostly up-right) position during procedures (Stephens, Barkey & Hall 1999:54; Sparks, Setlik & Luhman 2007:445)
• by giving the child as much control as possible during procedures (Steward et al. 1996:109; Armstrong 1992:211)
• adequate preparation (Nkoane & Oberholzer 2005:2,23; Kain et al. 2006:656).
Priority 8. Support with schoolwork (internal environment–mind–intellect)
Eiser (1998:629) appealed for the continuation of education through School Hospital Services or home teaching for children admitted in a haematology-oncology unit. Although the child does not feel well
enough to benefit academically most of the time, it can provide some continuity and assist the child in going back to school.McGrath (2001:232) as well as Varni et al. (1993:752) added that if
these children go back to school it creates some sense of normalcy which is essential for coping.
Priority 9. Alleviation of misconceptions and giving adequate information (internal environment–mind–intellect)
Von Essen et al. (2002:609) described information as ‘the most important aspect of care for children aged 7–13 years with cancer’. Van Veldhuizen and Last (1991:231) found that
children as young as four years coped better if they received adequate information about their cancer diagnosis from the start. Videos, films or slide shows (Brewer et al. 2006:14) or even interactive
computer programs (Bisignano & Bush 2006:72) can all be used, if available, to pass information on to the child and toprepare him or her for healthcare experiences.
Priority 10. The reduction of negative sensory stimulation from the environment and the normalising of the environment (external environment–physical)
Pangrazio (1999:79) mentioned the important aspects that should be taken into account when designing a hospital area for children. There should be areas where the child can play and move freely, as well
as variety in the design that will stimulate the child’s senses and some measures of control over the environment. There should be accommodation for family members, and there should be measures
of distraction as well as normalising the environment through music, scenes of natureand animals. According to Coad and Coad (2008:43), children are quite capable of rendering an input in the design
and colour used in a paediatric unit. It seems as if they prefer the paler range of colours with the blue-green colours on top of the list and themes representing water, nature, the beach and the sea.
Priority 11. Humour as intervention (internal environment–mind–emotion)
Humour is not usually discussed as part of the psychosocial support of children in hospital, yet was chosen in the eleventh place out of the 19 resources. Vagnoli et al. (2005) found a significant
reduction in anxiety of children who interacted with clowns before and during anaesthesia induction. At the Red Cross Children’s Hospitalin South Africa, the visits of clowns (called ‘Care
Clowns’) bring smiles and laughter to the children of the burns unit every week. UP, the nonprofit organisation that started the clown visits strives to encourage children to laugh at least
once a day, as they believe in the healing power of laughter (Laugh yourself better, 2004:52). Dowling (2002:125) mentioned other kinds of humour interventions beneficial to hospitalised children such
as gentle tickling, telling jokes, funny stories, poems andriddles, watching funny movies and rewarding patients with silly stickers.
Priority 12. Establishing a trusting relationship (external environment–social)
Gaynard et al. (1998:8) referred to a number of studies that confirmed that a supportive relationship with a member of the healthcare team significantly reduced achild’s emotional distress
and enabled him or her to cope better with the hospital experience. According to Gaynard et al. (1998:8), research has shown that a trusting relationship had a greater impact on reducing
children’s stress during hospitalisation than did the provision of information about the health care experience. This contradicts the results of the current study where the children chose
information as more important than a trusting relationship. Bricher (1999:452,453) stated that thetrust between a child and the nursing staff is continuously challenged as a result
of the invasive and often painful procedures that the staff has to perform, and it could be debated whether the children in the current study might be sceptical about establishing a trusting
relationship with someone in the healthcare team.
Priority 13: Tokens of appreciation and encouragement (internal environment–mind–emotion)
Several authors mentioned special stickers as gifts or some sort of tangible incentive after procedures (Ball & Bindler 2003:182; Björk, Nordström & Hallström 2006:216; Stephens et al.
1999:58; Redd 1989:576; Hedenkamp 1980:66). Liossi (2002:125) explained that a small trophy could be presented to the child as a ‘symbolof mastery’, acknowledging the fact that the child
did the best he or she could do during the procedure. She added that the goal was to change the meaning of the procedure for the child and to ‘persuade children to view it as a challenge, and
as an opportunity to master a difficult situation, thus resulting in positive feelings of self-efficacy and increased self-esteem’. Golden et al. (2006:1072) found that a small, inexpensive
toy given to children significantly reduced their anxiety and stressfulbehaviour during the administration of an oral premedication.
Priority 14. Animal assisted activities (external environment–social)
Although the Theory of Health Promotion in Nursing (University of Johannesburg: Department of Nursing Science 2009:7) defines the social environment as ‘human resources in the external
environment’ of the child, a significant bond could be established between an animal and the child. Kaminski, Pellino and Wish (2002:322) explained that animal interaction could promote
social interaction and behaviour, increase emotional comfort, decrease loneliness, boost self-esteem as well asestablish a sense of independence in a human being. According to these authors,
pets (especially dogs) are used in various healthcare settings such as intensive care units, long-term care facilities, clinics, children’s units as well as in psychotherapy. Odendaal
(2002:132–133) found that interaction with a dog can significantly decrease stress in a human being as indicated by a decrease in blood pressure and the stress hormone cortisol. However,
this is still a new and unfamiliar practice inSouth Africa and it might be possible that the children will regard animals as more important as they are become familiar with this practice (Table 2).
Priority 15. Literature (internal environment–mind–emotion)
The word ‘narrative’ means ‘listening to and telling or retelling stories about people and the problems in their lives’, and this perspective can be used effectively in therapy,
especially for children (Freeman, Epston & Lobovits 1997). In addition, bibliotherapy is used to help children cope with a real life problem by either reading to the child, or giving him or her a
relevant story to read (McIntyre 2004). Brett (1988:14) explained that stories could be used by anyone and may well assist childrenin coping with difficult situations through teaching them about
themselves and their problems and enabling them to experience feelings of comfort, support and understanding. It also enables the child to externalise the problem, therefore making it less threatening
and enabling the child to look at it more objectively (Freemanet al. 1997).
Priority 16. Music interventions (internal environment–mind–emotion)
Malan (2003:125) concluded that children with a haematology-oncology diagnosis chose to escape from difficult situations by listening to music. Music could reducepain postoperatively
(Good et al. 2005:240) as well as during invasive procedures (Colwell, Davis & Schroeder 2005:50; Dahlquist 1992:352; Klein & Winkelstein 1996:79). Longhi and Pickett
(2008:253) found that live soothing music resulted in a significant increase in oxygen saturation levels in long term paediatric patients. A music therapist working therapeutically
with children in a hospital could benefit the children tremendously, and Edwards (2005:36) described the role of a musictherapist as that of supporting children in hospital with regard
to pain management and assisting them to cope with psychological stress.
Priority 17. Play interventions (internal environment–mind–emotion)
Hall and Reet (2000:54) stated that all healthcare professionals should introduce play in their daily interaction with children as it aids in calming, communicating, reassuring and befriending children.
Kiely (1992:73) stated that one of the standard requirements for quality care in a paediatric unit is a comprehensive play program. As part of the play program, written procedures should be in place for
play equipment, toy safety, equipment storage, care and availability and hygieneprocedures such as disinfecting toys. There should be a protocol for toys used in isolation, locations should be identified
that are acceptable for group activities, and activity suggestions for groups and individuals should be in place so that volunteers and staff knew the correct procedures and all followed the same guidelines.
Different kinds of play activities could be encouraged (Gaynard et al. 1998:69), especially in regard to expressive play where the child can express his or her emotions,such as:
• Familiarisation activities so that the child could become familiar with the hospital.
• Dramatic play that not only serves to enable children to express themselves, but help them understand what is happening to them and consequently facilitates a feeling of control over their circumstances.
In addition, play assists staff in evaluating a child’s understanding of the healthcare experience.
• If playing is difficult for the child when he or she is too ill, injured or immobilised, he or she can benefit from watching others play for him or her.
Priority 18. Electronic devices (internal environment–mind–emotion)
Computer programs have been used successfully during preparation of children for procedures (Bisignano & Bus 2006:61), educating them about a certain disease(Krishna et al. 2006:75) as well as
for pain management (Pritchard 2005:2). Malan (2003:118) stated that watching television is a way to escape reality and a coping skill inherent to children, and television can even be utilised as an
effective distraction tool during invasive procedures (Cramer-Berness & Friedman 2005:96–97). Hopelab (2006) added that an interactive video game about cancer significantly increased
adolescents’ information about cancer as well as their self-efficacy. Children areaccused of spending too much time watching television or playing play-station or computer games; therefore
it is quite unexpected to find that children rate electronic devices as least important. This might be because they are often warned against the negative impact of these devices and it
could be speculated that they feel guilty when watching television or playing electronic games.
Priority 19. Promoting control (internal environment–mind–volition)
Armstrong (1992:210) explained that it was important for the long-term coping mechanisms of children with an oncology diagnosis to experience some control overcertain aspects of their treatment, such as
their daily routine as well as the routine during procedures. According to Li, Lopez, and Lee (2007:39), children would see a situation as less threatening if they believed that they have some control
over it. Van Veldhuizen and Last (1991:16) stated that if someone felt in control of a situation, it would lead to feelings of security, confidence, competence and power, whereas an experience of being
out of control would bring about feelings of anxiety, fear,helplessness and depression. It is, therefore, clear that it is important for the child in a haematology-oncology unit to experience some
control over the situation in order to feel less like a victim and to reduce the experience of negative emotions. However, Van Veldhuizen (1992:16) stated that children in a haematologyoncology unit
find themselves in a situation robbed of all feelings of control. Reed et al. (2003:72) added that all children admitted to hospital could experiencedisempowerment and loss of control as a
result of the fact that they were not always able to understand the situation and were often excluded from decision-making. Van Veldhuizen (1992:24) further explained that when a situation was
appraised as ‘resistant to change’, a person would resort to a secondary locus of control where they adapted and accepted the situation as unchangeable. This might explain why the
children chose promoting control as the lowest priority. It is likely that they haveadapted to a situation where they did not have any control and then viewed it as futile to even think
of the situation as being different or that they could have any control of the situation.
As a result of the broad scope of the research, in-depth investigations into the different resources were not possible and the current research merely scratched the surface of a very complicated field of
study. As pointed out previously, only children from the private sector were included in the study and because of the fact that the majority of children are admitted in public hospitals, the needs of children
in a haematology-oncology unit in public hospitals should also be explored as well as the resources that could address these needs.
Limited research has been conducted in South Africa pertaining to the psychosocial support of children in hospital and this is a field waiting to be explored furtherthrough research. Research should also
be encouraged in all the relevant disciplines such as psychology, education, social work and sociology. The following recommendations could be made regarding research areas needing urgent attention:
• the impact of hospitalisation on children in the South African context should be explored
• the impact of haematology-oncology treatment on children in the South African context should be explored
• new developments with regard to the psychosocial support of children in hospital in the South African context should be encouraged and monitored throughresearch
• each of the resources discussed for the purpose of this study should be explored further relating to the implementation of these resources in the South African context.
The results of this research can be utilised in nursing education in order to increase the awareness of the nursing students regarding the psychosocial support, not only of children in a haematology-oncology
unit, but also of children in general paediatric wards. Research conducted in South Africa in 1992 (Orr 1992:181)concluded that registered nurses in charge of paediatric wards lacked the necessary
knowledge concerning the emotional adjustment of children in hospital and 90.9% of the participants in the study indicated that they would want more information and training in this regard. The literature review from the current study provides valuable information with regards to resources that can be implemented in the clinical practice. It is recommended that at least one nurse
in the haematology-oncology unit is appointed with the exclusive function of taking responsibility for the implementation of the resources in that specific unit as it has been conducted in the unit
where the researcher works. This will ensure that the support of these children is a priority and willnot vanish in the rush of everyday nursing activities. It is also important to notice that when the prioritising of the resources according to their importance for the children was compared to the internal and externaldimensions of the child, it became
apparent that the first three resources, as chosen by the children, all concerned the external social environment of the child as explained by the Theory for Health Promotion in Nursing (University
of Johannesburg: Department of Nursing 2009:6). It could therefore be concluded that support from parents and other people of significance are important to the child and should be taken into account
in the psychosocial support of these children. One wayof ensuring that parents and other significant people are included in the support of children in a haematology-oncology unit is through partnerships.
According to Bishop (2000:6–7), a partnership entails equal relationships between the nurse, the child, the parents and family of the child and even between other members of the healthcare team.
Seeing that the spiritual dimension is the next priority, these partnerships should also include pastors, ministers and other spiritual counsellors.
Cadranel (1990:44) as well as Patenaude and Kupst (2005:13) stated that children in a haematology-oncology unit are all different and their responses are influencedby various factors such as personal
traits and discrepancies in the circumstances surrounding the sick child. However, a definite trend could be found in the way the children who participated in the field study responded to the request
to prioritise the resources. This confirms the notion that children are experts where it concerns their own experiences and valuable partners in research (Baumann 1996:27). It could therefore be
concluded that support from parents and other people ofsignificance are of the utmost importance to the child and should be taken into account first when facilitating support for children in a
haematology-oncology unit. It could also be concluded that children in a haematology-oncology unit do not experience sufficient control in their situation and this should be addressed in order
to ensure that children are adequately empowered in a haematology-oncology unit.
The Cancer association of South Africa (CANSA) contributed financially in support of this study. The names of the children were obtained from the ChildhoodCancer Foundation of South Africa (CHOC). Thank you to all the children who contributed to this research and to their parents who brought them to the interviews. Some of the children are not with us in thislife any more – may they be
remembered and honoured through this research.
Abramovitch, R., Freedman, J.L., Henry, K. & Van Brunschot, M., 1995, ‘Children’s capacity to agree to psychological research: knowledge of risks and benefits and voluntariness’,
Ethics and Behavior5(1), 25–48. doi:10.1207/s15327019eb0501_3
Alexander, K.W., Quas, J.A., Goodman, G.S., Ghetti, S., Edelstein, R.S., Redlich, A.D., Cordon, I.M. & Jones, D.P.H., 2005, ‘Traumatic impact predicts long-term memory for documented
child sexual abuse’, Psychological Science 16(1), 33–40. doi:10.1111/j.0956-7976.2005.00777.x,
PMid:15660849
American Academy of Pediatrics, 2001, ‘The assessment and management of acute pain in infants, children and adolescents’, Pediatrics
108(3), 793–797. doi:10.1542/peds.108.3.793, PMid:11533354
Armstrong, F.D., 1992, ‘Psychosocial intervention in pediatric cancer: A strategy for prevention of long-term problems’, in T.M. Field, P.M. McCabe & N. Schneideman (eds.), Stress
and coping in infancy and childhood, Lawrence Erlbaum, New Jersey.
Ball, J.W. & Bindler, R.C., 2003, Pediatric Nursing: Caring for children, 3rd edn., Prentice Hall, New Jersey.Battles, H.B. & Wiener, L.S., 2002, ‘Starbright World: Effects
of an electronic network on the social environment of children with life-threatening illnesses’, Children’s Health Care31(1),47–68.
doi:10.1207/S15326888CHC3101_4
Baumann, S.L., 1996, ‘Parse’s research methodology and the nurse researcher-child process’, Nursing Science Quarterly9(1), 27–32.
doi:10.1177/089431849600900108, PMid:8710300
Bishop, J., 2000, ‘Partnership in care’, in H. Langton (ed.), The child with cancer, pp. 1–20, Baillière Tindall, Edinburgh. Bisignano, A. & Bush, J.P., 2006, ‘Distress
in Pediatric hematology-oncology patients undergoing intravenous procedures: Evaluation of a CD-ROM intervention’, Children’s Health Care 35(1), 61–74.
doi:10.1207/s15326888chc3501_6
Björk, M., Nordström, B. & Hallström, I., 2006, ‘Needs of young children with cancer during their initial hospitalization: an observational study’, Journal of Pediatric Oncology
Nursing 23(4), 210–219. doi:10.1177/1043454206289737, PMid:16766686
Brett, D., 1988, Annie stories, Workman Publishing, New York.
Brewer, S., Gleditsch, S.L., Syblik, D., Tietjens, M.E. & Vacik, H.W., 2006, ‘Pediatric anxiety: Child Life intervention in day surgery’, Journal of Pediatric Nursing 21(1), 13–22.
doi:10.1016/j.pedn.2005.06.004, PMid:16428010
Bricher, G., 1999, ‘Paediatric nurses, children and the development of trust’, Journal of Clinical Nursing, 8, 451–458.
doi:10.1046/j.1365-2702.1999.00275.x, PMid:10624262
Burke, R.V., Kuhn, B.R. & Peterson, J.L., 2004, ‘Brief report: A “storybook” ending to children’s bedtime problems – The use of a rewarding social story to reduce
bedtime resistance and frequent night walking’, Journal of Pediatric Psychology 29(5), 389–396. doi:10.1093/jpepsy/jsh042,
PMid:15187177
Burns, N. & Grove, S.K., 2003, Understanding nursing research, Saunders, Pennsylvania.
Burns, N. & Grove, S.K., 2009, The practice of nursing research: Appraisal, Synthesis and generation
of evidence, 6th edn., Elsevier, St Louis. Cadranel, J., 1990, ‘The child patient’s perception of cancer’, Maternal and child health, February, 44–47.
Carver, C.S. & Scheier, M.F., 1996, Perspectives on personality, 3rd edn., Allyn & Bacon, Boston.
Child Life Council, 1997, Guidelines for the development of Child Life Programs, 2nd edn., Child Life Council, Rockville.
Coad, J. & Coad, N., 2008, ‘Children and young people’s preference of thematic design and colour for their hospital environment’, Journal of Child Health
Care 12(1), 33–48. doi:10.1177/1367493507085617, PMid:18287183
Colwell, C.M., Davis, K. & Schroeder, L.K., 2005, ‘The effect of composition (art or music) on the self-concept of hospitalized children’, Journal of Music Therapy 42(1), 49–63.
PMid:15839732
Cook, J.L. & Cook, G., 2005, Child development: Principles and perspectives, Pearson Education, Boston.
Cramer-Berness, L.J. & Friedman, A.G., 2005, ‘Behavioral interventions for infant immunizations’, Children’s Health Care34(2), 95–111.
doi:10.1207/s15326888chc3402_2
Cutland, S., 2004, A team approach to the immuno-compromised child, Nursing Update 28(8), 38–40.
Dahlquist, L.M., 1992, ‘Coping with aversive medical treatments’, in A.M. La Greca, L.J. Siegel, J.L. Wallander & C.E. Walker (eds), Stress and coping in child health, pp. 345–376, Guilford Press, New York.
Derevensky, J.L., Tsanos, A.P. & Handman, M., 1998, ‘Children with cancer: an examination of their coping and adaptive behavior’, Journal of Psychosocial Oncology 16(1),
37–61.
Dowling, J.S., 2002, ‘Humor: A coping strategy for pediatric patients’, Pediatric Nursing 28(2), 123–132. PMid:11962177
Du Toit, S.J. & Kruger, N., 1991, Die kind: ‘n Opvoedkundige perspektief, Butterworths, Durban.
Edwards, J., 2005, ‘A reflection on the music therapist’s role in developing a program in a children’s
hospital’, Music Therapy Perspectives 23(1), 36–44.
Eiser, C., 1998, ‘Practitioner review: Long-term consequences of childhood cancer’, Journal of Child Psychology
and Psychiatry 39(5), 621–633. doi:10.1111/1469-7610.00362,
PMid:9690926, doi:10.1017/S0021963098002583, PMid:9690926
Freeman, J., Epston, D. & Lobovits, D., 1997, About narrative therapy with children,viewed 07 March 2006, from www.narrativeapproaches.com/narrative%20papers%20folder/papers.htm
Gaskill, M., 2001, ‘Nourishing the soul: pediatric center invites patients, families to explore spiritual aspects of care’, Nurse Week, viewed 07 October 2004, from
http://www.nurseweek.com/news/features/01-01/pedi.asp
Gaunt, J., 1993, ‘Promoting family health: Architects can make a difference in children’s healthcare by designing sensitive, family-centered environments’, Architecture,
April, 33–34. PMid:10125167
Gaynard, L., Wolfer, J., Goldberger, J., Thompson, R.H., Redburn, L. & Laidley, L., 1998, Psychosocial care of children in hospitals: A clinical practice manual from the ACCH Child
Life Research project, Child Life Council, Rockville.
Gizynski, M. & Shapiro, V.B., 1990, ‘Depression and childhood illness’, Child and Adolescent Social Work Journal, 7(3), 179–197.
doi:10.1007/BF00755312
Golden, L., Pagala, M., Sukhavasi, S., Nagpal, D., Ahmad, A. & Mahanta, A., 2006, ‘Giving toys to children reduces their anxiety about receiving premedication for surgery’,
Anesthesia and analgesia102, 1070–1072. doi:10.1213/01.ane.0000198332.51475.50
Good, M., Anderson, G.C., Ahn, S., Cong, X. & Stanton-Hicks, M., 2005, ‘Relaxation and soothing music help post-op patients control pain’, Research in Nursing and Health
28, 240– 251. doi:10.1002/nur.20076
Hall, C. & Reet, M., 2000, ‘Enhancing the state of play in children’s nursing’, Journal of Child Health Care4(2), 49–54.
doi:10.1177/136749350000400201, PMid:11855399
Hedenkamp, E.A., 1980, ‘Humanizing the intensive care unit for children’, Critical Care Quarterly 3(1), 63–73. PMid:10246628
Hobbie, W.L. Stuber, M., Meeske, K., Wissler, K., Rourke, M.T., Ruccione, K., Hinkle, A. & Kazak, A.E., 2000, ‘Symptoms of posttraumatic stress in young adult survivors of childhood
cancer’, Journal of Clinical Oncology, 18(24), 4060–4066. PMid:11118467
Hopelab, 2006, Re-Mission outcome study: A research trial of a video game shows improvement in health-related outcomes for young people with cancer, viewed 11 July 2006, from
www.hopelab.org/docs/Outcomes%20Study.pdf
Kain, Z.N., Mayes, L.C., Caldwell-Andrews, A.A., Karas, D.E. & Mcclain, B.C., 2006, ‘Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing
surgery’, Pediatrics118(2), 651–658. doi:10.1542/peds.2005-2920, PMid:16882820
Kaminski, M., Pellino, T. & Wish, J., 2002, ‘Play and pets: The physical and emotional impact of Child-Life and pet therapy on hospitalized children’, Children’s Health Care
31(4), 321–335. doi:10.1207/S15326888CHC3104_5
Kaufman, K.L., Harbeck, C., Olson, R. & Nitschke, R., 1992, ‘The availability of psychosocial interventions to children with cancer and their families’, Children’s Health
Care 21(1), 21–25. doi:10.1207/s15326888chc2101_3
Kiely, A.B., 1992, Volunteers in child health: Management, selection, training and supervision, Association for the Care of Children’s Health, Bethesda.
Klein, S.A. & Winkelstein, M.L., 1996, ‘Enhancing pediatric health care with music’, Journal of Pediatric Health Care
10(2), 74–81. doi:10.1016/S0891-5245(96)90030-9
Kortesluoma, R., Hentinen, M. & Nikkonen, M., 2003, ‘Conducting a qualitative child interview: Methodological considerations’, Journal of Advanced Nursing 42(5),
434–441. doi:10.1046/j.1365-2648.2003.02643.x, PMid:12752864
Krishna, S., Balas, E.A., Francisco, B.D. & König, P., 2006, ‘Effective and sustainable multimedia education for children with asthma: A randomized controlled trial’,
Children’s Health Care35(1), 75–90. doi:10.1207/s15326888chc3501_7
Laugh yourself better, 2004, Nursing Update 28(8), 52.
Levine, P.A. & Kline, M., 2007, Trauma through a child’s eyes: Awakening the ordinary miracle of healing; Infancy through adolescence, North Atlantic Books, Berkeley.
Li, H.C.W., Lopez, V. & Lee, T.L.I., 2007, ‘Psychoeducational preparation of children for surgery: The importance of parental involvement’, Patient Education and Counselling
65(1), 34–41. doi:10.1016/j.pec.2006.04.009, PMid:16872785
Lin, T., Chang, K., Liu, S. & Chu, H., 2006, ‘A persuasive game to encourage healthy dietary behaviours of kindergarten children’, in National Taiwan University, viewed 19 August 2006,
from http://mll.csie.ntu.edu.tw/papers/persuasion_ubicomp2006.pdf
Liossi, C., 2002, Procedure-related cancer pain in children, Radcliffe Medical Press, Oxon.
Longhi, E. & Pickett, N., 2008, ‘Music and well-being in long term hospitalized children’, Psychology of Music 36(2), 247–256. doi:10.1177/0305735607082622
Malan, M., 2003, ‘Coping skills of the oncology child: An educational psychological perspective’, M Ed Thesis, Dept. of Education, University of South Africa, Pretoria
McCaffrey, C.N., 2006, ‘Major stressors and their effects on the well-being of children with cancer’, Journal of Pediatric Nursing
21(1), 59–66. doi:10.1016/j.pedn.2005.07.003, PMid:16428015
McDermott Sales, J., Fivush, R., Parker, J. & Bahrick, L., 2005, ‘Stressing memory: Long-term relations among children’s stress, recall and psychological outcome following
hurricane Andrew’, Journal of Cognition and Development, 6(4), 529–545. doi:10.1207/s15327647jcd0604_5
McGrath, P., 2001, ‘Findings on the impact of treatment for childhood acute lymphoblastic leukaemia on family relationships’, Child and Family Social
Work 6, 229–237. doi:10.1046/j.1365-2206.2001.00200.x
McGrath, P.J., Dick, B. & Unruh, A.M., 2003, ‘Psychologic and behavioral treatment of pain in children and adolescents’, in N.L. Schechter, C.B. Berde & M. Yaster,
Pain in infants, children and adolescents, 2nd edn., pp. 303–316, Lippincott Williams & Wilkins, Philadelphia.
Mcintyre, T., 2004, Bibliotherapy, viewed 05 July 2006, from www.behavioradvisor.com/Biblio.html
Meltzer, L.J. & Rourke, M.T., 2005, ‘Oncology summer camp: benefits of social comparison’, Children’s Health Care 34(4), 305–314.
doi:10.1207/s15326888chc3404_5
Morison, M., Moir, J. & Kwansa, T., 2000, ‘Interviewing children for the purpose of research in primary care’, Primary Health Care Research and Development, 1:113–130.
doi:10.1191/146342300675316801
Nkoane, M.M. & Oberholzer, A.E., 2005, ‘Assessing and managing the needs of the infant/child patient’, in A. Young (ed), Juta’s Manual of Nursing Health Care Priorities,
pp.2/1–2/36, Juta, Cape Town.
Nolan, T., 1996, ‘Traditional scientific designs and ethics’, in J. Daly (ed), Ethical intersections: Health research, methods and researcher responsibility, pp. 58–65,
Allen & Unwin, Australia.
Odendaal, J., 2002, Pets and our mental health, Vantage Press, New York.
Oncology Nursing Society, 2005, Chemotherapy and biotherapy guidelines and recommendations for practice, 2nd edn., Oncology Nursing Society, Pittsburg, viewed 19 August 2006, from
http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=8337&nbr=4665
Orr, J., 1992, ‘A nursing model for the total care of the hospitalized preschool child’, MA Thesis, Dept. of Nursing, University of South Africa, Pretoria.
Pangrazio, J., 1999, ‘Healing environments’, in B.K. Komiske (ed.), Designing the world’s best: Children’s Hospitals, pp. 79–122, Images Publishing, Australia.
Patenaude, A.F. & Kupst, M.J., 2005, ‘Psychosocial functioning in pediatric cancer’, Journal of Pediatric Psychology
30(1), 9–27. doi:10.1093/jpepsy/jsi012, PMid:15610981
Petrovic, P., Petersson, K.M., Ghatan, P.H., Stone-Elander, S. & Ingvar, M., 2000, ‘Pain-related cerebral activation is altered by a distracting cognitive task’,
Pain 85, 19–30. doi:10.1016/S0304-3959(99)00232-8
Phipps, S., Fairclough, D., Tyc, V. & Mulhern, R.K., 1998, ‘Assessment of coping with invasive procedures in children with cancer: State-trait and approach-avoidant dimensions’,
Children’s Health Care 27(3), 147–156. doi:10.1207/s15326888chc2703_1
Potts, N.L. & Mandleco, B.L., 2002, Pediatric Nursing: Caring for children and their families, Delmar, New York.
Pritchard, C., 2005, ‘Virtual reality games help children manage pain’, Medical Post, Toronto 41(7), 2.
Range, L.M. & Cotton, C.R., 1995, ‘Reports of assent and permission in research with children: Illustrations and suggestions’, Ethics and Behavior
5(1), 49–66. doi:10.1207/s15327019eb0501_4
Redd, W., 1989, ‘Behavioral interventions to reduce child distress’, in J.C. Holland & J.H. Rowland (eds.), Handbook of psycho-oncology: Psychological care of the patient with
cancer. Oxford University Press, Oxford.
Reed, P., Smith, P., Fletcher, M. & Bradding, A., 2003, ‘Promoting the dignity of the child in hospital’, Nursing Ethics
10(1), 67–76. doi:10.1191/0969733003ne540oa, PMid:12572762
Siegel, M., 1995, ‘More than words: the generative power of transmediation for learning’, Canadian Journal of Education
20(4), 455–475. doi:10.2307/1495082
Siegel, M., 2006, ‘Rereading the signs: Multimodal transformations in the field of literacy education’, Language Arts 84(1), 65–77.
Slade, A., 2000, ‘Impact of treatment on the family’, in H. Langton (ed.), The child with cancer, 105–139, Baillière Tindall, New York.
Sparks, L.A., Setlik, J. & Luhman, J., 2007, ‘Parental holding and positioning to decrease distress in young children: A randomized controlled trial’, Journal of
Pediatric Nursing 22(6), 440–447. doi:10.1016/j.pedn.2007.04.010,
PMid:18036464
Stephens, M.E., Barkey, M.E. & Hall, H.R., 1999, ‘Techniques to comfort children during stressful procedures’, Advances in Mind-Body Medicine 15, 49–60.
PMid:10955974
Steward, M.S., O’Connor, J., Acredolo, C. & Steward, D.S., 1996, ‘The trauma and memory of cancer treatment in children’, in M.H. Bornstein & J.L. Genevro (eds.),
Child development and behavioral paediatrics, Lawrence Erlbaum, New Jersey.
Tadmore, C.S. & Ben Arush, M.W., 2000, ‘Changes in the policies of the Department of Hematology, 1982–1998, designed to promote the mental health of children with leukaemia and
enhance their quality of life’, Pediatric Hematology and Oncology 17, 67–76. doi:10.1080/088800100276677
Trochim, W.M.K., 2006, Scaling, viewed 11 October 2008, from http://www.socialresearchmethods.net/kb/scaling.php
Twycross, A., Moriarty, A. & Betts, T., 1998, Paediatric pain management: A multi-disciplinary approach, Radcliffe Medical Press, Oxon.
University of Johannesburg: Department of Nursing., 2009, Paradigm, University of Johannesburg, Johannesburg.
Vagnoli, L., Caprilli, S., Robiglio, A. & Messeri, A., 2005, ‘Clown doctors as a treatment for preoperative anxiety in children: A randomized, prospective study’, Pediatrics
116(4), e563–e567, viewed 09 November 2005, from http://pediatrics.aappublications.org/cgi/contents/full/116/4/e563
Van Dalen, V. (National Health Program Coordinator, CANSA), 23 April 2008, Personal interview with A. E. Oberholzer.
Van Dongen-Melman, J.E.W.M. & Sanders-Woudstra, J.A.R., 1995, ‘Psychosocial aspects of childhood cancer: A review of the literature’, in J.E.W.M. Van Dongen-melman (ed.),
On surviving childhood cancer: Late psychosocial consequences for patients, parents and siblings, Koninklijke Bibliotheek, Den Haag.
Van Veldhuizen, A.M.H., 1992, ‘Emotional distress and control strategies’, in B.F. Last & A.H.M. Van Veldhuizen (eds.), Developments in Pediatric psychosocial
Oncology, pp. 15–37,Swets & Zeitlinger, Amsterdam.
Van Veldhuizen, A.M. & Last, B.F., 1991, Children with cancer: Communication and emotions, Swets & Zeitlinger, Amsterdam.
Varni, J.W., Katz, E.R., Colegrove, R. & Dolgin, M., 1993, ‘The impact of social skills training on the adjustment of children with newly diagnosed cancer’, Journal of Pediatric
Psychology18(6), 751–767. doi:10.1093/jpepsy/18.6.751, PMid:8138868
Von Essen, L., Enskär, K., Haglund, K., Hedström, M. & Skolin, I., 2002, ‘Important aspects of care and assistance for children 0–7 years of age being treated for cancer’,
SupportiveCare in Cancer 10, 601–612. doi:10.1007/s00520-002-0383-y, PMid:12436218
White, M.A., Williams, P.D., Alexander, D.J., Powell-Cope, G.M. & Conlon, M., 1990, ‘Sleep onset latency and distress in hospitalized children’, Nursing Research 39(3),
134–139. doi:10.1097/00006199-199005000-00002, PMid:2342897
Woodgate, R.L., 2006, ‘The importance of being there: Perspectives of social support by adolescents with cancer’, Journal of Pediatric Oncology Nursing 23(3), 122–134.
doi:10.1177/1043454206287396, PMid:16624888
Woods, N.F. & Catanzaro, M., 1988, Nursing research: Theory and practice. Mosby Company, St Louis.
|
